Case Studies

Real Stories. Practical Takeaways. A Path Back to Headspace.
Fog of Mind is about creating headspace and supporting healthier personal and working environments. The case studies below share real experiences of mental health challenges and recovery, including what the fog felt like, what helped, and the practical takeaways that can support others. If you are struggling, you are not alone, and there are steps you can take.
Case Study 1: When the Fog Rolled In (Anxiety and Depression)
The story
I did not wake up one morning and decide I was unwell. It arrived in small, believable pieces.
A knot in my stomach. A persistent feeling of unease. A strange homesickness I could not explain. I kept telling myself it was stress, tiredness, just a phase, anything except what it was. There is no playbook for this. Not one that arrives on time, anyway.
At my worst, I genuinely thought I was going mad.
The signs I missed
Looking back, the warning lights were flashing for a while, I just did not know what they were:
- That constant “something is wrong” feeling, even on a normal day
- Tightness in my stomach, like my body was bracing for impact
- A shrinking confidence, even in things I was usually good at
- Feeling disconnected from people, even when surrounded by them
- Thinking that everyone else was coping better than me
The hardest part was not the symptoms themselves. It was the confusion. The not-knowing. The fear that this was just my new normal.
The diagnosis and the relief
Eventually, I saw a psychiatrist and was diagnosed with general anxiety disorder and moderate to severe depression.
Oddly, the diagnosis brought relief. Not because it was pleasant to hear, but because it gave the chaos a name. I was not broken. I had a condition. And importantly, it was treatable.
That moment matters. When you are in it, you do not need vague reassurance. You need something solid: clarity, a plan, and support.
When I hit the floor
My mood dipped and stayed low. My confidence drained away. My cognitive ability deteriorated to the point where simple decisions felt heavy and my mind felt unreliable.
That was the floor.
If you have been there, you will know what I mean. It is not dramatic. It is flat. Grey. A kind of emotional exhaustion where even basic tasks feel like a climb.
Some days were harder than others. And the panic attacks were horrendous. They are frightening, physical, and convincing. In the moment, it can feel like your body is shouting that you are not safe, even when you are.
What helped me climb back up
Recovery was not one magical fix. It was a handful of practical supports, stacked up over time.
1) Walking with my dog, Mr Sox
A small routine of walking Mr Sox around the shores of Rutland Water. Fresh air. Movement. A reason to leave the house, which was not easy. The simplest habits can become the handrail that keeps you steady.
2) Blogging
Writing gave me somewhere to put the noise. It helped me make sense of what I was feeling, and it reminded me I still had a voice, even when my confidence was low.
3) Medication (prescribed)
For me, a daily dose of 20mg citalopram was part of my treatment. Medication is personal and should always be discussed with a qualified clinician, but I include it here because it was a genuine part of my pathway.
4) Hard sessions on my road bike
I am not claiming exercise “cures” anything. I am saying it helped me. The sheer intensity gave me a clean outlet and, over time, built a sense of capability again. I've been a Tour de France calibre rider, but I know how to ride hard and fast, and that's exactly what I did.
5) Time
This might be the most underrated piece. I improved over nine months, not nine days. Progress was real, but it was not linear.
Case Study 2: When Experience Helps: Walking Someone Home from the Edge
The story
Mike (not his real name) was a former soldier, like me. When I arrived in the team he was resentful. Partly because he wanted my role, one he had applied for but did not even get an interview.
Winning him over took time and patience. A lot of negotiating, a lot of consistency, and a clear message shown through action rather than talk. That is what leaders do. You build trust through positive action, even when it starts from a difficult place.
Before I joined, Mike had a nasty accident in a brand new vehicle. There was significant damage, but apart from Mike’s ego, nobody was hurt.
A few months later my supervisor rang me. She sounded distressed.
“Mike’s had an accident. He’s sat in the cab literally shaking.”
I paused. “I am on my way.”
When I saw Mike on that grey morning in Barnsley, I saw a carbon copy of myself from a few years earlier. If you have read Case Study 1, you will understand what I mean. The look. The fear. The physical shake that is not about cold.
I recognised the signs, but I am not a doctor. In that moment the job was not diagnosis. The job was support and safety.
So we did the simple, important things.
- We got Mike home.
- We informed HR.
- We informed transport that Mike would not be driving for a while.
- I told the chain of command, calmly and clearly, not to expect Mike back for months. I said six months to err on caution.
Some people may think that is dramatic. I did not. I had seen what happens when pressure is added to an already overloaded system.
My supervisor and I visited Mike just before Christmas. He had been off work for about six weeks and he looked like hell. I remember thinking, quietly, that this is how I must have looked back in 2013 (Case Study 1).
Mike eventually returned to work. He had been prescribed 20mg of citalopram and diagnosed with general anxiety disorder and moderate to severe depression.
I have never taken recreational drugs, but there is an old saying that a drug user can spot a drug user. In the same way, someone who has lived with anxiety can recognise it quickly in others. I deal with anxiety most days. I can see the symptoms a mile off.
What I learned
This case study is not about being a hero. It is about being useful.
The takeaway is that I provided Mike with empathy, and I created space for him to stabilise without shame. That was my role.
It was up to Mike, with professional support, to connect the other two sides of the Mental Health Triangle: motivation and time.
Later, my boss told me people were thankful for the way I dealt with Mike, because they would have struggled.
I replied, honestly, that I was no magician. Walking in his shoes made it easier to know what to do next.
Key takeaways from Mike's Story
- You do not need to be a clinician to spot someone in distress. You need to respond with care and common sense.
- In workplaces, early action protects the person, the team, and the wider system.
- Empathy is not sympathy. It is practical support, calm communication, and removing unnecessary pressure.
- Leaders set the tone. If you treat mental health as something to hide, people will hide until they break.
- Lived experience can be a strength, especially when it helps you act with clarity and kindness.
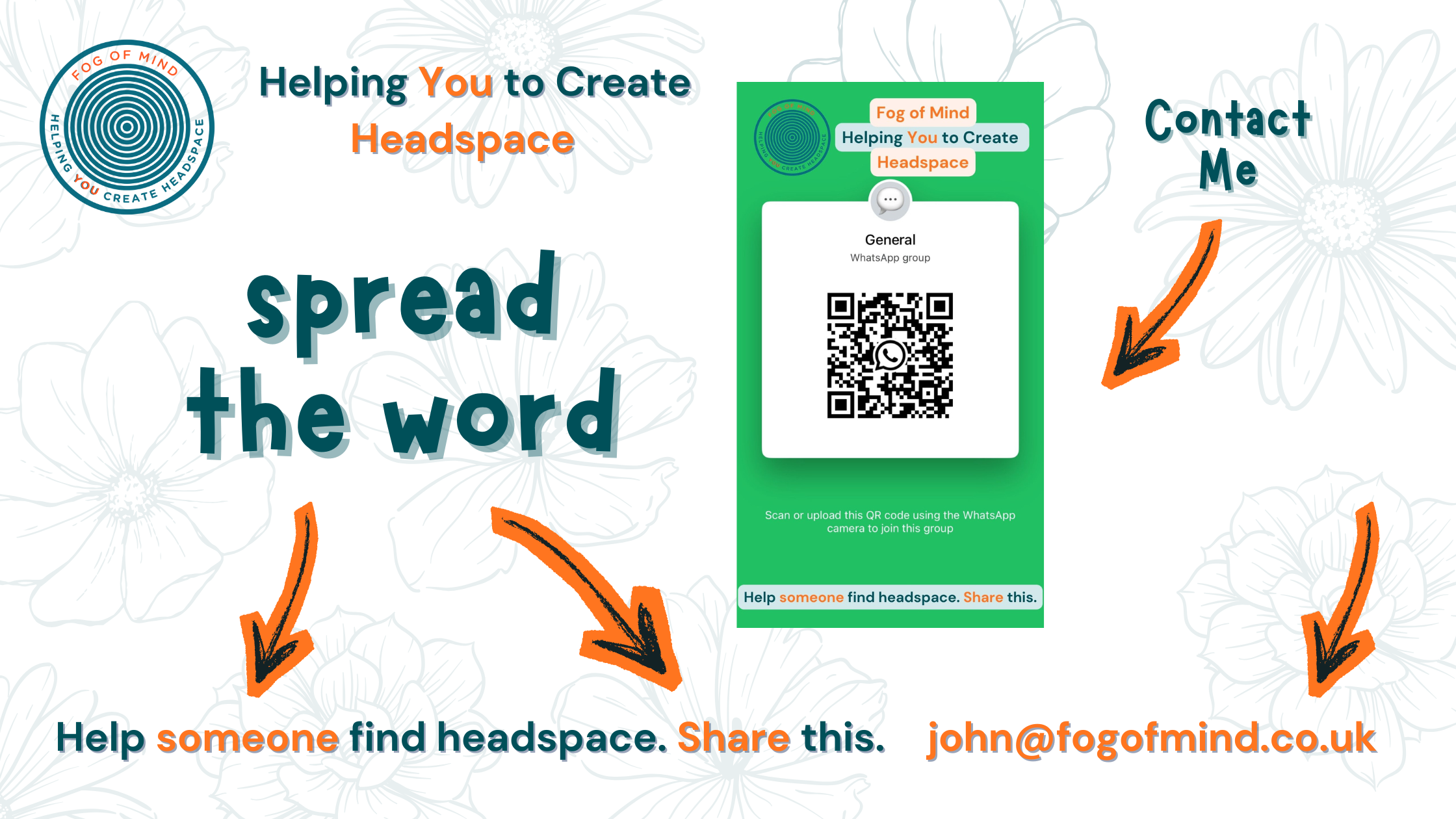
Help someone find headspace. Share this.
The Mental Health Triangle
Over time, I started to think about recovery and support as a triangle. Three sides that hold you up:
1) Motivation
Not hype. Not forced positivity. Realistic motivation that helps you take the next small step when you would rather do nothing.
2) Time
Time to rest, time to process, time to heal, time away from relentless pressure. Without time, everything becomes urgent, and urgent is where anxiety thrives.
3) Empathy
People struggling with mental health do not need sympathy. They need empathy. A loved one, a friend, or a line manager who can say:
“I do not fully understand what this feels like, but I am here, and I am listening.”
If any side of that triangle is missing, things get harder fast. You can push through for a while, but you will feel the wobble.
Key takeaways
- If you feel “off” for weeks, do not wait for a crash to take it seriously.
- Asking for help is not weakness. It is a skill. Remember, it's ok to ask for help!
- If asking feels too big, start by finding coping strategies that buy you breathing space.
- Empathy beats sympathy every time, especially in families and workplaces.
- Recovery is possible, even when it does not feel like it. I have walked this path.
How Fog of Mind fits in
Fog of Mind exists because I know what it is like to be stuck in that grey space, unsure what is happening and unsure how to explain it.
If any part of this story feels familiar, Fog of Mind can support you through:
- 1:1 conversations focused on perspective, coping strategies, and next steps
- Talks and workshops for teams and organisations, aimed at building healthier working environments
- Practical frameworks, like the Mental Health Triangle, that make it easier to talk about what is going on

Call to action: If you want to talk, find me on WhatsApp and tell me what you are dealing with. One honest message is enough to start.